11/03/2022
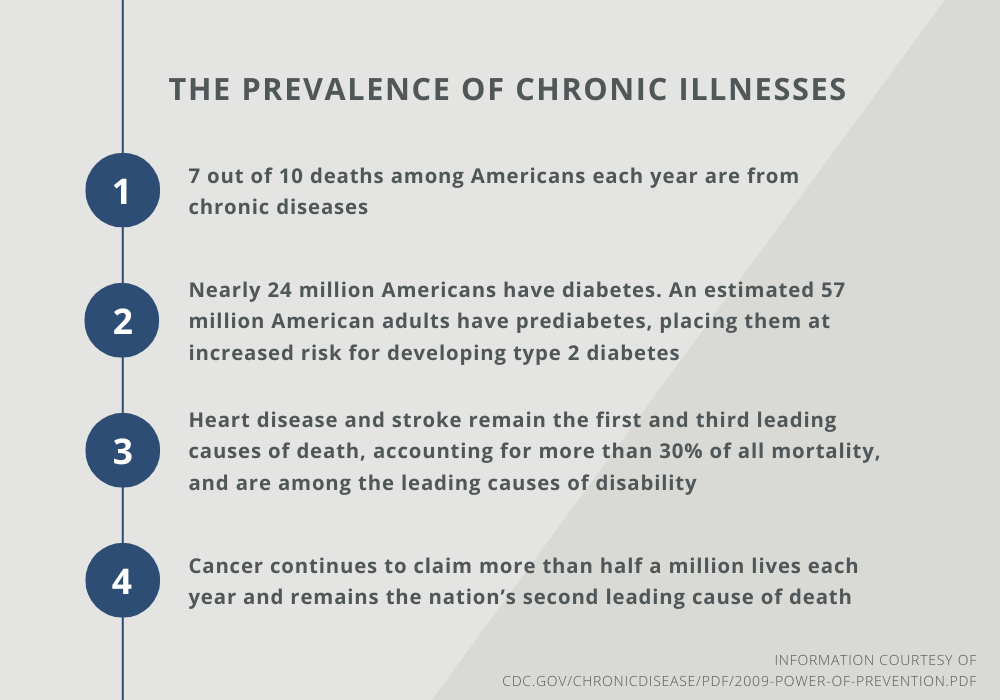
According to the CDC, more than 75% of U.S. healthcare expenditures are for chronic conditions such as heart disease, cancer, and diabetes. In several cases, these common and costly conditions can be preventable. This begs the question: Shouldn’t we take charge of patient health before preventable conditions become a costly problem?
 Shifting your organization from a reactive to a proactive healthcare model could yield substantial benefits not only for your organization but for your patients as well. Unfortunately, this isn’t an easy, overnight shift. However, by focusing on managing and leading the transformation to a proactive healthcare organization, you can position your people and processes to meaningfully adopt a new standard of patient care.
Shifting your organization from a reactive to a proactive healthcare model could yield substantial benefits not only for your organization but for your patients as well. Unfortunately, this isn’t an easy, overnight shift. However, by focusing on managing and leading the transformation to a proactive healthcare organization, you can position your people and processes to meaningfully adopt a new standard of patient care.
What is Proactive Care?
At its core, proactive healthcare empowers patients to take charge of their health through lifestyle changes and data collection. These lifestyle changes and additional data points, like daily heart rate or minutes exercised, enable healthcare providers to identify chronic conditions early and establish a thorough care plan. This requires a proactive relationship between patients and providers based on their current age, lifestyle, and habits. Leveraging a proactive healthcare model early in a patient’s journey will generate better health outcomes for the patient and positive financial impacts for the healthcare system.
What is Reactive Care?
Traditionally, medicine is practiced in a “reactive” way, where providers intervene to interrupt the progression of an established diagnosis. Reactive services for these patients will always be a critical part of the care model. However, there are many patients with preventable chronic conditions that are currently treated in the same reactive way. If a condition is preventable – or even mitigable –why are we letting it cause patient, provider, and resource strain?
Shifting from Reactive to Proactive Patient Care
In the 1960s, early discussions about how computers and technology could revolutionize the healthcare industry were met with resistance. Today, computers, phones, tablets, and watches are all key to the patient’s journey in gathering data, storing records, and communicating. Similar to this revolution, proactive care has been met with adoption resistance due to the burden it puts on healthcare providers, clinical staff, and patients to change their current practices. How can a healthcare system successfully shift its mindset to being more proactive? It should develop a well-defined organizational change management approach to ensure adoption across the board.
With any change, an organization must take a careful, methodical approach to ensure successful adoption and integration. Here are a few steps health systems can take today to lay the foundation for the transformation to a proactive model:
1. Understand your patient makeup. One of the first steps in any change journey is to understand your stakeholders and learn what they are doing today. Leveraging data and analytics to understand patient outcomes, usage patterns, and population health information is a critical step when defining what types of proactive care would be most utilized. Additionally, gaining contextual insights on the patient’s experience and perception of the brand will also be invaluable. Establishing patient feedback forums and focus groups is a great way to gather insights that can’t be gleaned from analytics reports.
2. Reinforce proactive care through targeted communication and training practices. There’s truth behind the old adage that something needs to be communicated seven times before it’s understood. That’s why it’s imperative to bring your impacted stakeholder groups along for your proactive care change journey. Start by communicating the “why” behind the shift to a proactive care model and using examples, including the benefits of the change, to gain their buy-in. Training your clinical staff on the proactive care “why” will empower them to reinforce the messaging to their patients and peers.
3. Build a stronger rapport with your patients. From the welcome desk to the exam room to the lab to the final check-out station, your nurse practitioners, MDs, clinical staff, and administrators are creating bonds with your patients. Over time, these bonds create patient and provider trust. For example, if a doctor suggested lifestyle changes at one visit and the patient is seeing results by the follow-up appointment, there’s a new opportunity to build trust. The doctor can trust that this patient will follow their recommendations, while the patient can trust that the doctor’s orders will yield results. In the future, this can translate to increased patient accountability and fewer appointments, as the preventative care recommendations the doctor makes are more likely to stick. Recognizing this opportunity to create trust-based change is a key organizational change management principle.
These are a few steps your healthcare system can take today to start the transition into a proactive care model, but there are many more proven change practices and principles to support true adoption. While reactive care will always be a critical practice, proactive care is the future.
Are you ready to take advantage of the innovative and transformational healthcare world we live in today? Fill out the form below to connect with one of our consultants.