HealthcareAI
The AI arms race in healthcare: Innovation without compromise
There are several key factors that healthcare organizations should consider when it comes to keeping up with the race…
Read article

Healthcare Process Improvement
01/25/2023
by L, en Oster and Brooke Przilas

Landen Oster, BSN, RN joined Sendero in the summer of 2022 with an extensive background in the healthcare field. Landen, a registered nurse by background, has spent time working for a leading healthcare analytics company and is currently completing his MBA with a concentration in healthcare administration.
Brooke Przilas, MBA joined Sendero in the summer of 2021 after spending more than six years working for a large Texas-based healthcare system, where one of her primary focus areas was optimizing hospital and outpatient operations.
Recently, these Senderoans were catching up over a cup of coffee and discussed some of the key challenges they faced while working in the clinical setting. To their surprise, they found many similarities and shared themes, even though they had worked in different roles in different healthcare organizations. This realization led to a deeper conversation, review, and study surrounding various models of nurse staffing.
A 2021 analysis by Premier Inc., a longtime leader in healthcare, noted that in our post-pandemic world, the healthcare industry is paying $24 billion more in labor costs than that of pre-pandemic requirements. While this has since started to trend downward, the significant spend on labor and associated costs, including overtime, agency resources, and increased sick time, still emphasizes the need for healthcare organizations to re-evaluate their current nurse staffing models. Doing so will empower organizations to glean opportunities for optimizing resource utilization and leverage team-based care.
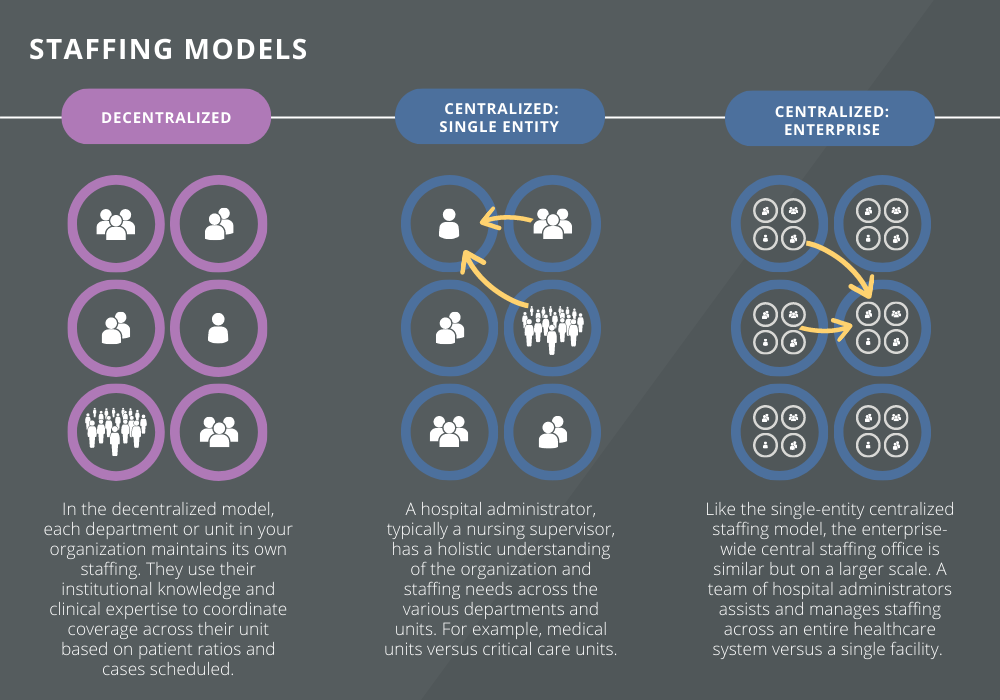
This blog highlights three primary nurse staffing models: (1) decentralized nurse staffing, or those where each unit or department maintains its own staffing, and centralized nurse staffing, including both (2) single-entity and (3) an enterprise-wide central staffing office, where resources and resource planning are shared across the organization, providing support for all nursing units.
The nurse staffing model you implement can ultimately impact labor costs, retention, patient outcomes, and organizational culture.
Decentralized Nurse Staffing Model
A decentralized nurse staffing model leverages deep unit-based knowledge and skill sets to support specific patient and provider needs. This model can be ideal for procedure areas and units, where nurses develop and maintain a specific and unique knowledge of processes and provider preferences. Oftentimes, staff can anticipate the next steps in a procedure based on previous experience, which could be difficult for a nurse who is floating. For example, scheduling coordination for your cardiac catheterization lab could be primarily supported by the department supervisor, who has a unique understanding of provider preferences, procedure details, and patient flow based on direct experience within the cardiac specialty.
Centralized Nurse Staffing Model
For units outside of specialty procedure areas, a centralized nurse staffing model is widely considered the more comprehensively efficient staffing model with unique benefits, including:
Single Entity: One scenario where this model is effective is when a department, say oncology, is understaffed for a shift. At the same time, the post-critical care unit at the same hospital may have several empty beds and is looking to send a nurse home. Instead of having an oncology nurse work overtime or call in an additional resource, the nurse from the post-critical care unit could float to the oncology department. The float nurse is able to assist the oncology unit with their staffing challenges and the unit can save on overtime or on-call costs. Additionally, the float assignment gives the nurse experience with a different patient population, allowing them to sharpen their skills and become more well-rounded in their expertise.
On a larger scale, many large healthcare systems have implemented the enterprise-wide central staffing office in which, similar to the single entity model, a specialized nurse could float from one hospital to another to assist and reduce the staffing deficit for that hospital and unit. This high-level view of available staff allows for transparency across the system and provides insight into where staff is needed, while also being strategic in reducing overhead costs.
With both the single-entity and enterprise-wide centralized staffing models, the largest benefit is the improved nurse-patient staffing ratios, ultimately providing a safer environment of care for the patient and improving the overall bottom line of the organization. Many studies have concluded that inadequate nurse-patient staffing ratios contribute to the increased prevalence of safety events. Through both centralized staffing models, hospital leadership gain greater insight into staffing needs across the organization and can repurpose staff to units, meeting the needs of the communities they serve while being mindful of overhead expenses.
As we’ve outlined the key benefits and considerations to exploring the adoption of a new nurse staffing model above, our ultimate goal is to provide a flexible, long-term solution that reduces labor costs, maintains a safe and efficient organization, and addresses staffing shortages and organizational culture. While a centralized nurse staffing model can easily appear to be the gold standard with its potential for cost savings and improved workplace culture, we understand this model isn’t ideal for every facility. A highly specialized surgery center with a team upholding unique training and educational requirements across procedures, for example, may realize greater benefits in maintaining or adopting a decentralized nurse staffing model where resource-sharing is not practiced or available. It’s important to take your specific operational needs and goals into account when identifying opportunities to enhance the effectiveness of your nurse staffing model.
Steps to Consider When Evaluating Your Organization’s Nurse Staffing Model
1. Conduct a current state assessment. A robust current state assessment and documentation of the present operational circumstances and how they impact your organization is critical when beginning this evaluation.
2. Evaluate the possibilities. Think about how each of the proposed models would impact your clinical staff. This analysis should evaluate the models and their alignment with your strategic goals and individual needs and nuances of your organization.
3. Implement the new model effectively. Often seen as the most difficult part, a sound execution with a well-defined expected staffing process is essential. Change management considerations are a huge part of this last step. Change fatigue is real, and a major contributor to workforce burnout. Establishing the “why” behind any new program updates is the first step in gaining employee buy-in and change adoption.
Not sure where to start? Our consultants can walk with you, step by step, in transforming your nurse staffing model to one that is not only operationally efficient, but also supports your team in providing high-quality, safe, patient-centered care.
Business insights
HealthcareAI
There are several key factors that healthcare organizations should consider when it comes to keeping up with the race…
Read article

Healthcare
While private equity investment in healthcare is valuable, providers should familiarize themselves with alternative…
Read article

HealthcareOptimize Technology
Advancements in health tech have allowed both patients and clinicians to experience the benefits of digital…
Read article